The laryngectomy
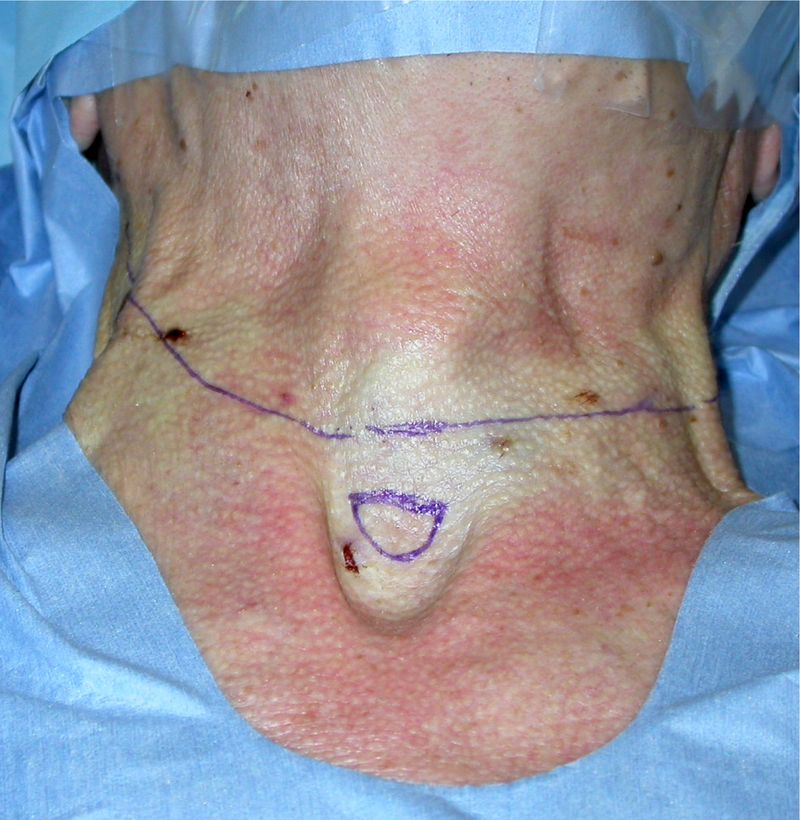
An incision is made from the mastoid tip across the cricoid cartilage of the larynx over to the opposite side.
An additional circular incision can be made in the jugular fossa for the tracheostoma which will follow. The separate circular incision encourages wound healing and helps to prevent scar distortion of the tracheostoma. It also makes it easier to supply tracheostoma adhesives. The diameter of the circular incision for the tracheostoma should be approximately the same as that of the trachea.
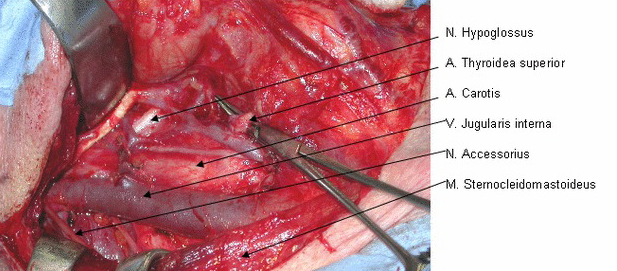
Mobilization of the skin is followed by the neck dissection on both sides of the neck. Nerves, blood vessels and muscles are spared as much as possible during the neck dissection and only removed if they are infiltrated by tumor.
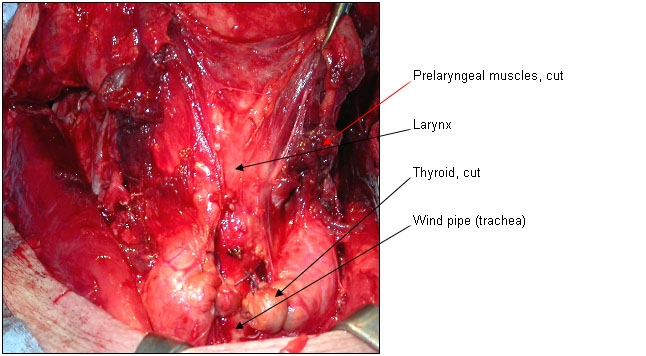
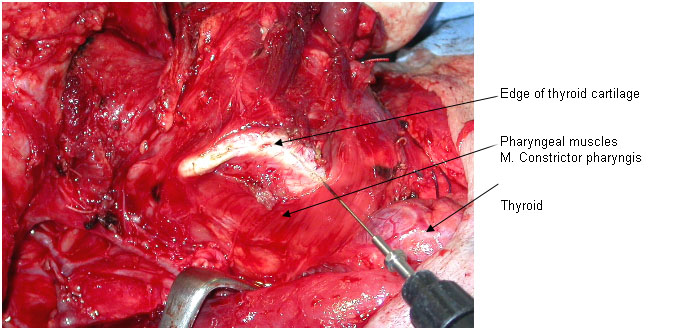
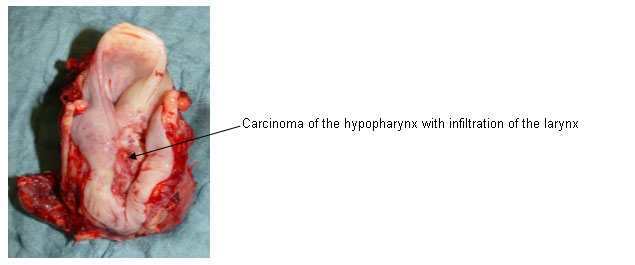
The hyoid bone is separated from the muscles to cranial. The Arteria laryngea superior and accompanying nerve (N. laryngeus superior) are cut through. The pharyngeal muscles (M. constrictor pharyngis) are cut through on the side of the thyroid cartilage. If the pharynx (hypopharynx) is not affected by the tumor, then it can be partly removed from the larynx and retained.
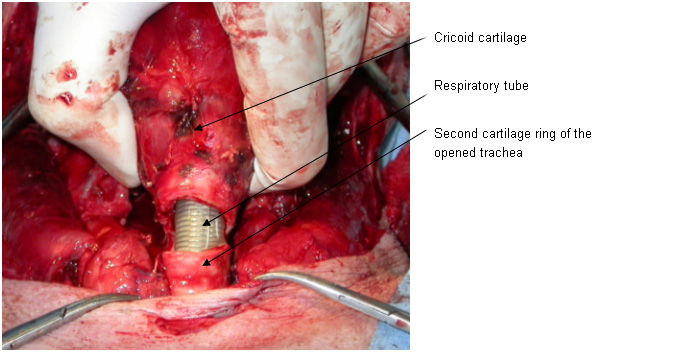
If the tumor has not extended to caudal into the wind pipe, then the wind pipe is cut through between the first and second tracheal rings. The second tracheal ring should remain completely intact and stable. After cutting through the membranous tracheal back wall (Pars membranacea), the first remaining ring is sewn in a circle into the tracheostoma incision. The cartilage tension of the intact tracheal ring keeps the tracheostoma open and prevents excessive shrinkage at a later stage. Since the wind pipe is sewn tightly to the skin, healing of the tracheostoma is much quicker.
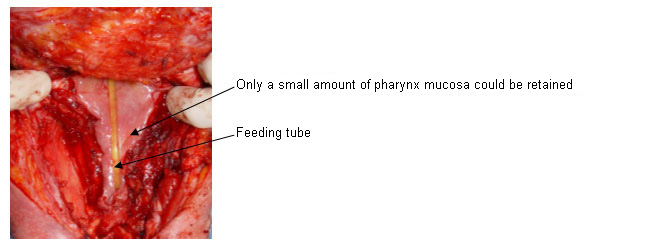
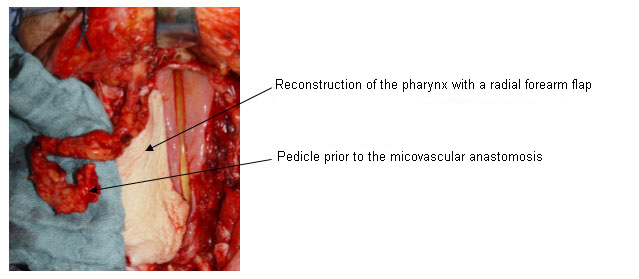
The opening of the hypopharynx is followed by cutting around the tumor, with visual control of the tumors margins if possible, and removal of the larynx. Extensive resections of the hypopharynx and prior radio chemotherapy should be followed by a wide-lumen reconstruction of the hypopharynx. Much consideration is then given to the indication for flap surgery, for instance with a free radial forearm flap or a pectoralis flap. This will prevent problems with swallowing occurring later as the result of scarred stenosis (narrowing) of the neopharynx (the newly created pharynx).
Next step is the placement of a voice prosthesis
Furthermore a unilateral myotomy (cutting through muscle) of the constrictor pharyngis muscles (muscles of the pharynx) and a same side neurectomy (cutting through nerves) of the pharyngeal plexus of the N.glossopharyngeus should be carried out before the pharynx is closed.
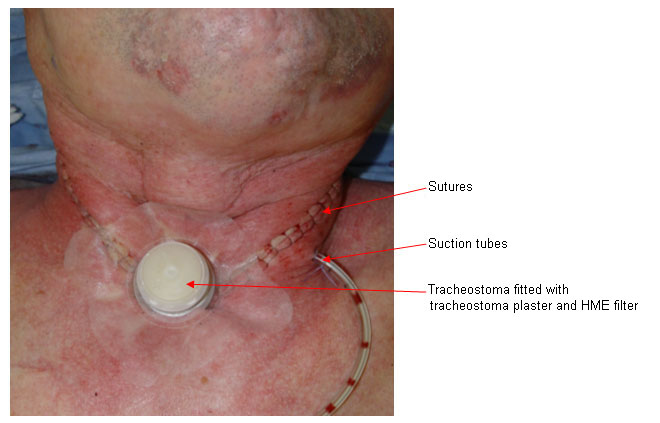
This is followed by the double-layered pharynx closure using inverted sutures. The constrictor muscles are not sewn back together again, as this would render the myotomy useless and make speaking very difficult. Careful double-layer closure of the pharynx reduces the rate of pharyngeal fistulas (disturbances to healing with saliva flow). The skin of the neck is sutured once a drainage has been inserted.
It is not essential to insert a tracheal tube at the end of the surgery. If bleeding stops well and the tracheostoma is stable, a tracheostoma adhesive with an HME filter may be applied at the end of the operation (less irritation and coughing). If healing progresses well, foods may be reintroduced and speech rehabilitation commenced after 8-10 days.