HME
Apart from the tracheostoma and financial difficulties, pulmonary symptoms (coughing, discharge, shortness of breath, breathlessness) are the main reasons for the reduction in the patient’s quality of life after a total laryngectomy.
The pulmonary symptoms occur as the result of the surgical short circuit of the upper airways (nose, sinuses, throat) when the tracheostoma is made. The functions of the nose are eliminated, as are the moistening, warming and filtering of the air (conditioning) breathed and the not insignificant resistance in the upper airways that is important for the development of the alveoli. A functioning upper respiratory tract can warm the air, almost independently of the external conditions, to 36-37°C and humidity to 100% by the time it reaches the trachea. It is difficult to quantify the filtering capacity of the nose. We are usually amazed by the contents of our handkerchief when we blow our nose after completing a dusty, dirty task! If this preparation (conditioning) of the airways does not take place, it will have serious consequences for the wind pipe, the bronchial tubes and the lungs themselves.
Examinations of the bronchial mucosa of mechanically ventilated patients (in whom the upper respiratory tract had also been short-circuited by the endotracheal tube), already revealed serious damage to the ciliated epithelia just a few hours after breathing recommenced with unconditioned room air. The ciliated epithelia no longer cleaned the airways adequately, and there was a build-up of secretions. The loss of moisture makes these secretions more viscous, and it is more difficult to cough them away.
In mechanical ventilation, special filters (HME filters = heat and moisture exchangers) are used that retain the warmth and moisture in the air breathed by the patient and prevent damage to the bronchial mucosa.
If even just a few hours of artificial ventilation with room air can cause irreversible damage to the bronchial mucosa, how much more important is it to protect the bronchial mucosa of a patient with a tracheostoma who will depend for the rest of his life on the direct inhaling of room air?
Protecting the bronchial tubes and lungs, pulmonary rehabilitation after a total laryngectomy, is the main aim, the non plus ultra, in the rehabilitation of the laryngectomee. From a purely medical consideration, pulmonary rehabilitation is far more important than learning to talk again – even though not many patients would agree with this.
Patients who do not also undergo pulmonary rehabilitation directly after laryngectomy will usually experience the typical development of the pulmonary systems. Directly after the laryngectomy, the low airway resistance when breathing through the tracheostoma is initially perceived as pleasant. However, very soon even a slightly increased breathing resistance, for instance when breathing through an HME, is perceived as unpleasant (which is why an HME should be placed on the tracheostoma directly after the laryngectomy whilst the patient is still in the operating theatre). Patients then go on to develop chronic bronchitis from the cold, dry air, which irritates the bronchial tubes and causes irreversible damage to the bronchial mucosa. Frequent coughing and phlegm are typical symptoms. The reduced breathing resistance encourages the development or worsening of pre-existing lung diseases (COPD, emphysema etc.). Typical emergencies include breathing difficulties and shortness of breath. Next, the pulmonary symptoms also lead to psychosocial symptoms such as a withdrawal from social activities, fear and depression. This association has been clearly confirmed in a number of studies.
In order to prevent the development of pulmonary and psychosocial symptoms following total laryngectomy, HMEs were also developed for laryngectomees as well as voice prostheses. Consistent use of HMEs has been proven to result in a massive reduction in pulmonary and psychosocial symptoms, and is recommended unreservedly. HMEs are available in lots of shapes and by lots of manufacturers. To this day there are no objective comparison tests of their effectiveness. So as a general rule: any HME is better than none!
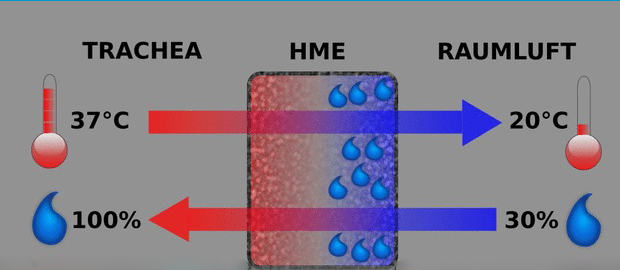
HMEs work to the following principle:
exhaled air flows through the HME, giving off warmth and moisture to the HME that it then stores. When inhaling, air flows through the HME in the opposite direction. It now passes the stored warmth and moisture over to the inhaled air, which is then warmed and moistened.
In order to use an HME efficiently, it needs to be airtight against the tracheostoma, as otherwise air will flow past the HME with the resulting loss of warmth and moisture. Most HMEs fit on a 22-mm connector so they can be attached to tracheostomy tubes, tracheostoma plasters and tracheostoma buttons.