Primary placement of a voice prosthesis
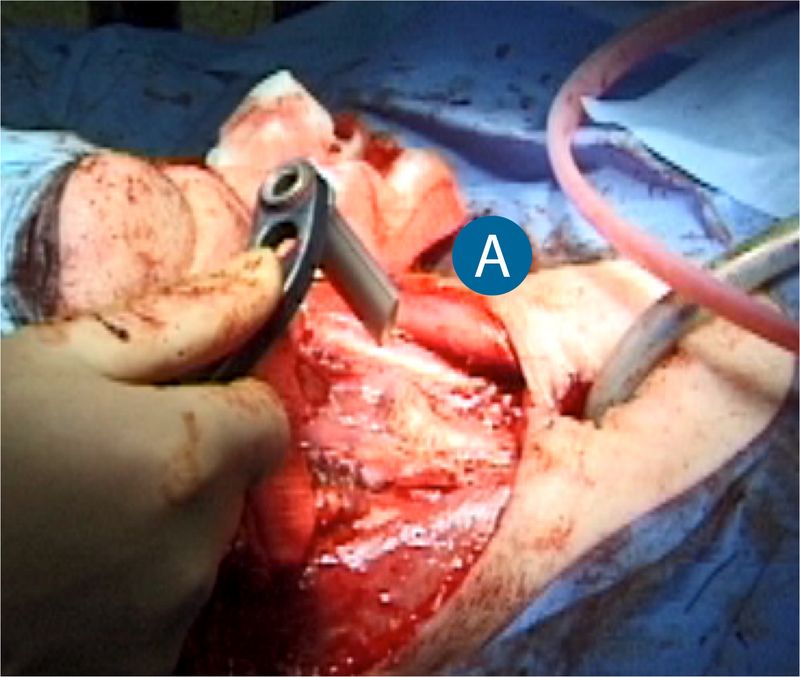
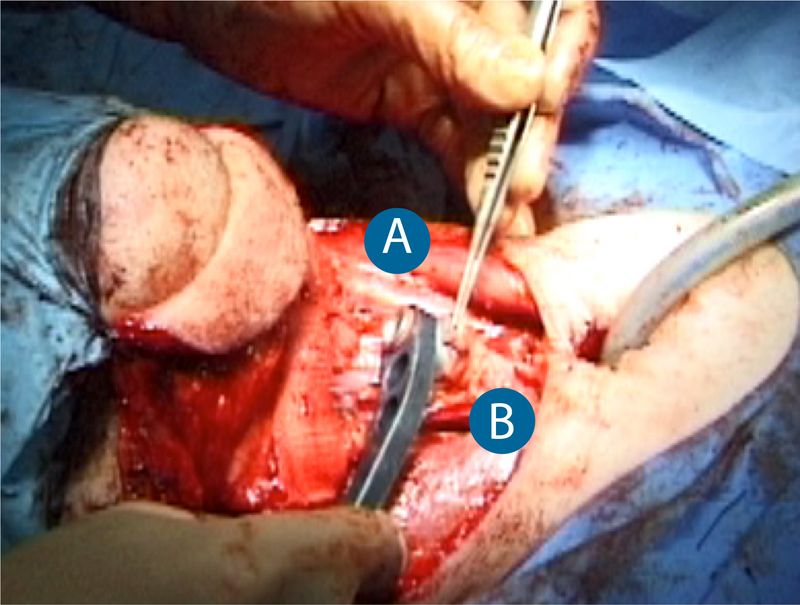
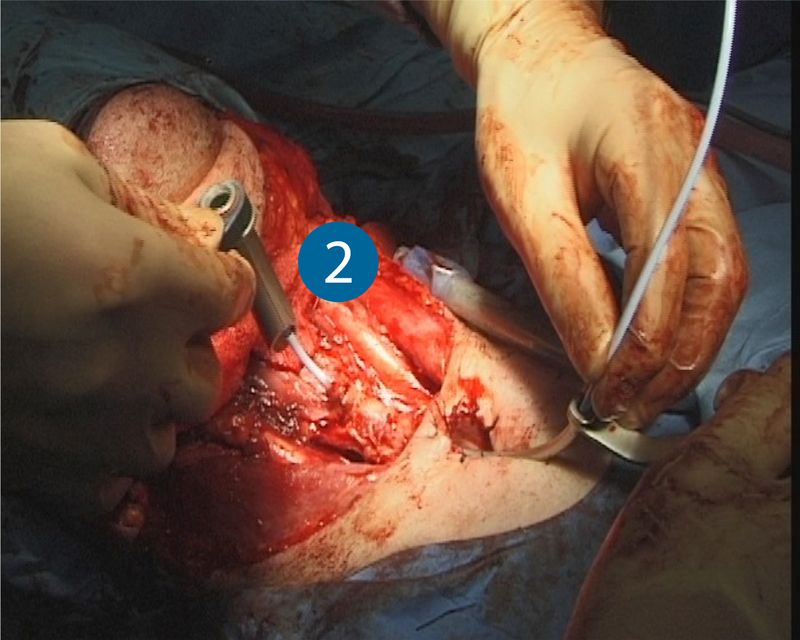
A voice prosthesis can usually be placed at the same time as the laryngectomy is carried out (primary placement). The primary insertion of the voice prosthesis is performed after the resection of the larynx and before the pharynx is closed. The tracheostoma should also have been completely sutured. This means the insertion point of the voice prosthesis can be determined with absolute precision. The puncture set after Hilgers is used to puncture the Pars membranacea of the trachea approx. 1 cm distal of the upper edge of the tracheostoma into the esophagus (shunt creation). A deeper puncture brings with it the risk of the shunt being very low down in the trachea, making it much more difficult to change the voice prosthesis, as the shunt often sinks a little further while the wound is healing. In order to prevent injury to the esophageal back wall by the puncture trocar (1), a pharynx protector is inserted in the open pharynx and upper food pipe before the puncture is performed. The puncture is then performed in the pharynx protector.
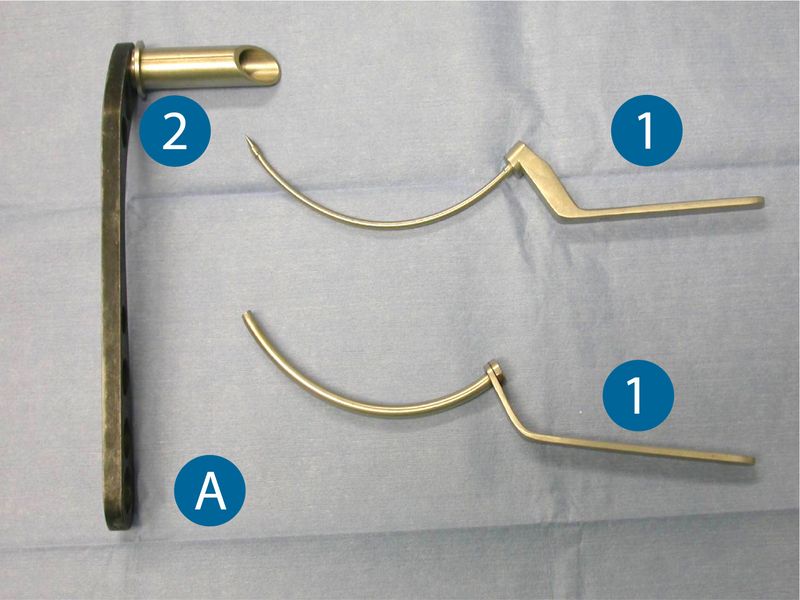
Instruments – trocar and pharynx protector after Hilgers
1) Two-part trocar (outer tube and puncture trocar)
A) Provox® pharynx protector
B) The pharynx protector is inserted in the entrance to the pharynx/esophagus
C) Cranial edge of the tracheostoma
D) Tip of the trocar at the puncture point 1 cm caudal to the upper edge of the tracheostoma
E) Ideal puncture point for shunt insertion
In order to allow the puncture of the trachea into the esophagus (it is quite likely to close spontaneously) to become a stable esophagotracheal fistula, a spacer or voice prosthesis needs to be inserted while the wound is healing. The insertion of a voice prosthesis in the newly punctured shunt is demonstrated on the following pages.
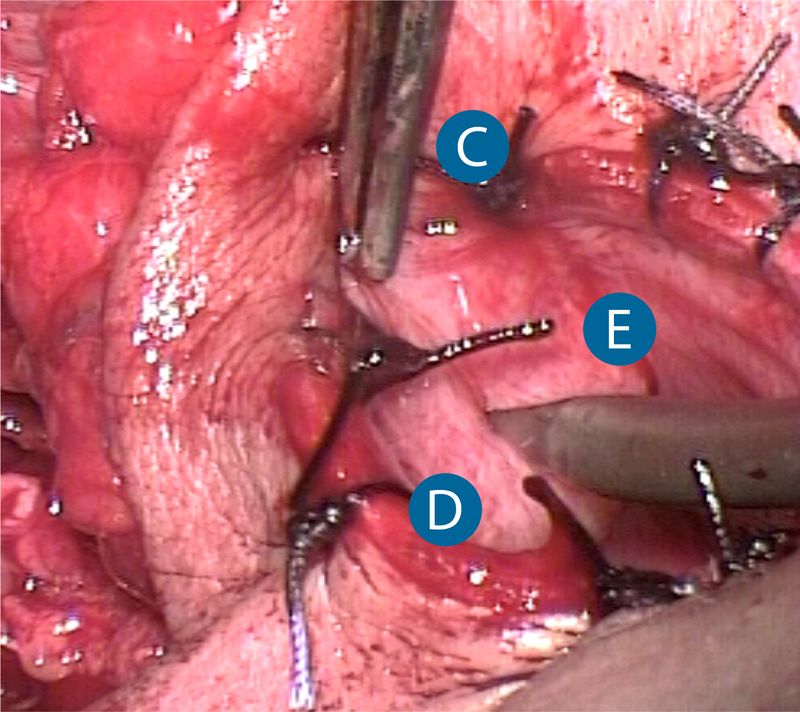
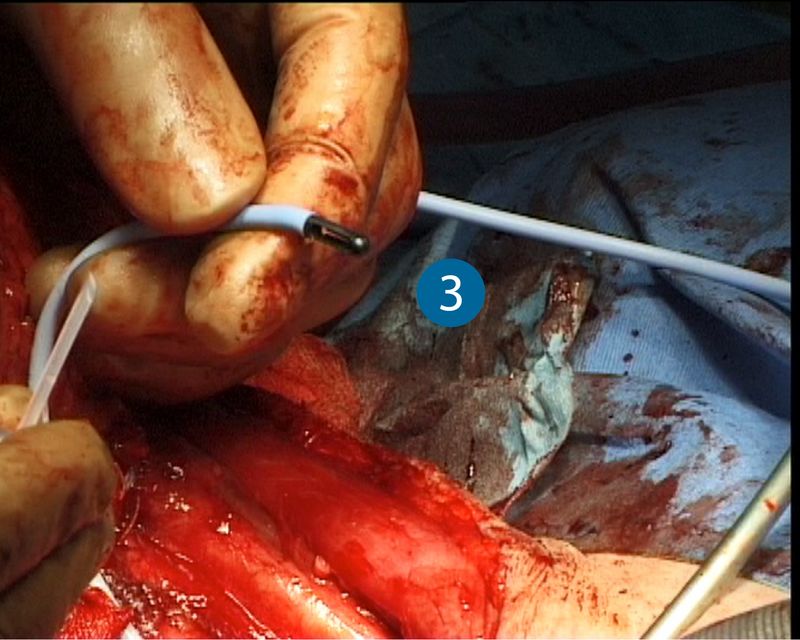
Once the puncture has been performed in the pharynx protector, the pointed trocar is removed. The outer tube remains in the puncture and pharynx protector. A guide wire is now pushed through the outer tube into the pharynx and through the pharynx protector. The pharynx protector is removed when the tip of the guide wire is visible in the pharynx. A voice prosthesis is attached to the tip of the guide wire and pulled retrograde into the shunt. The outer tube of the puncture trocar is also removed.
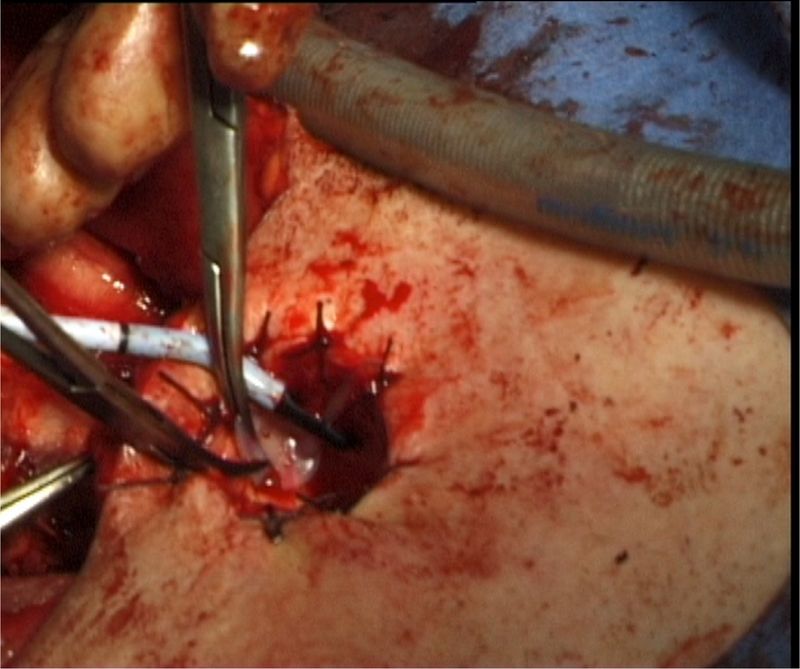
Now the tracheal flange of the voice prosthesis is pulled into the wind pipe, which is much more difficult with a freshly punctured shunt than with one that has healed. The unfolding of the tracheal flange of the voice prosthesis into the trachea is best achieved with two alternating anatomical clamps (4) and a gentle tug on the flange.
A prosthesis with a shaft length of 10 mm is usually sufficient for patients of normal weight and those who have not received prior radiation treatment. Shorter prostheses should not be used for the primary placement, as post-operative edema could cause them to cut into the flesh, which could lead to necroses.
Radiated or adipose patients should be given a prosthesis with a minimum shaft length of 12 mm.
The area of the wound will swell post-operatively, so the position of the voice prosthesis is checked on a daily basis in order to recognize pressure ulceration and necrosis promptly. If in any doubt, a longer voice prosthesis will have to be inserted shortly after surgery. Once wound healing has progressed to the extent that the patient is able to swallow, voice training may commence (if healing is normal, this is usually around the 10th day post-operative).